Sunday, December 23, 2007
EMR Video demos
Medications and History:
Using Dragon with eClinicalWorks
Ink-able Forms
Prescribing
Ordering Labs
Reviewing Labs
Tuesday, December 18, 2007
Finally a National Patient Identifier ?
Finally someone has has the guts to challenge the assumption that a national patient Identifier is not possible. Currently, we are forced to do algorithmic gymnastics in order to match a patient correctly, and even then, are at best 90% effective. This has led to the dependence on high priced MPI solutions.
The problem will only get worse as more health IT infrastructure is deployed. From a safety standpoint, 90% is not acceptable. Allowing patients to "opt-in" for use of a national patient Id is a great way to address any possible privacy concerns.
Tuesday, December 11, 2007
PHR Standards
Health insurers, HL7 team to create portable PHRs
Its nice to hear that HL7 is developing a PHR standard, however, I wonder if companies like Microsoft (see HealthVault) will the ones to create a de-facto, practical PHR standard that one can actually implement using existing tool sets. From my own experience with HL7 v3, I don't have much confidence that standards committees can put together something that is practical in implementation. See my previous post on HL7 v3 implementation.
Sunday, December 9, 2007
Telemedicine Provider: Interactive Care
I like the impressive demo that they have on their website. One of their key strengths is their integration to EMRs.

Health Information Technology in Massachusetts Forum
I recently attended this forum held in downtown Boston last week. The purpose of the form was to discuss the states role in health information technology adoption. There was an impressive panel made up of the top Healthcare IT leaders of the state, who also happen to be leaders at the national level as well. This panel included John Glaser, Ph.D; John Halamka, MD, Micky Tripathi and Janet Marchibroda.
The full list of speakers included: Secretary JudyAnn Bigby, MD; David Blumenthal, MD; Ray Campbell, Chris Gabrieli; John Glaser, Ph.D; John Halamka, MD; Jay Himmelstein, MD; Phil Johnston; Janet Marchibroda; John McDonough; Sen. Richard Moore; James Roosevelt, Jr.; and Micky Tripathi.
Here are some points made by the speakers at the forum which I found relevant:
Chris Gabrieli, Chairman of the Board Massachusetts Health Data Consortium
Chris worked for an EMR company in 1981 as part of a pilot. This system actually had decision support and clinical alerting. However when the pilot was completed, the medical clinic did not want to pay to have the system. As a result, the EMR equipment taken out of the clinic and the project was scrapped.
He spoke about the importance of patients being able to have a seamless transition when moving between healthcare providers. He compared it to how we can switch seamlessly from one cell phone provider to another while maintaining the same phone number.
John Glaser, Ph.D, CIO Partners HealthCare
Spoke about the need to broadly adopt healthcare IT technology.
The digital divide that is developing between the large hospitals/physician groups and the smaller healthcare organizations.
Partners Healthcare’s Telehealth programs and the benefits realized in managing CHF patients.
The need to get healthcare data exchanges up-and-running by aligning financial incentives between organizations.
Mentioned that MA-SHARE has gone as far as it can go and that now it needs broader support
Mickey Tripathi, CEO Mass eHealth Collaborative
EMR is a seen as a pure cost currently. The actual return on investment is seen much later.
Benefits of an EMR play out in a complicated manner over time. This is the reason why it's hard to establish a return on investment for EMRs using conventional methodologies.
John Halamka MD, CIO CareGroup Health System, and Dean for Technology at Harvard Medical School, CEO MA-SHARE
Spoke about the difficulties faced in trying save waste from the healthcare system by eliminating redundancy: "One man's redundancy is another man's country club".
Spoke of the problems of sustainability for RHIOs. He talked about how health-care providers will not pay if there is no infrastructure. In other words healthcare providers do not see the health information exchange as an investment. The challenge is how to build the infrastructure without the capital. John implied that the providers would see value and pay if there is a live health information exchange.
Janet Marchibroda MBA , Chief Executive Officer of the eHealth Initiative
The greatest challenge to RHIOs is building sustainability.

She mentioned that based on a recent survey on health information exchanges, the largest source of revenue is now coming from hospitals, not government grants.
The health information exchanges that are operational are exchanging Lab data, emergency department and outpatient clinical summaries.
Byron Byfield has written about the event on his blog.
Tuesday, December 4, 2007
Nursing homes will be facing greater scrutiny
There has been a lot of attention paid to quality of care in hospitals and outpatient settings with the use P4P and HEIDIS performance measures, and this has led to a proliferation of IT in these care settings. Unfortunately, nursing homes have lagged in adoption of technology. What is needed at the nursing homes, is the implementation of technology in order to improve the quality of care. I believe the time has come.
Thursday, November 22, 2007
Benefits of Telemedicine
Savings of $4.28 billion annually
Fierce Health had some interesting comments on this.
More related items:
California-Could-Become-National-Model-for-Telemedicine
California is the apparent leader in telemedicine. CA will be working on important issues such as reimbursement.
CITL Research
Telehealth Technologies Report Good discussion on the savings and benefits of telemedicine in various care settings: nursing homes, hospitals, correctional facilities etc.
Wednesday, November 21, 2007
Email Management
receives nearly 600 email a day ! All of which he says are legitimate. John also responds to all of his emails the same day!
Certainly, with the few emails that I have exchanged with John, he always got back to me the same day. He describes in his blog the rules he uses to go through all his emails. I found his method very useful, and have started using some of his techniques in my own email management strategy.
No Payment for Medical Errors: Massachusetts takes the Pledge
The types of medical errors that will not be reimbursed are:
•Surgery on wrong body part
•Surgery on wrong patient
•Wrong surgical procedure
•Unintended retention of a foreign object
•Patient death or serious disability associated with air embolism that occurs while being treated in a health care facility
•Patient death or serious disability associated with a medication error
•Patient death or serious disability associated with a hemolytic reaction due to administration of incompatible blood or blood products
•Artificial insemination with the wrong donor sperm or wrong egg
•Infant discharged to the wrong family.
This list will be expanded according to the article as more experience is gained in implementing this policy. I did not see much Grey in the list, its fairly black and white. These are all events which are definite errors. Where there may problems, would be in the case of wounds and infections. In these cases, its hard to know if an error actually led to the adverse event. This is the "Grey" area where the implementation of this policy could be problematic.
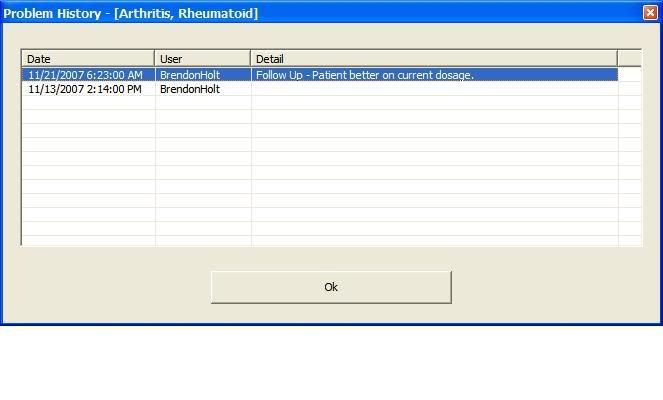
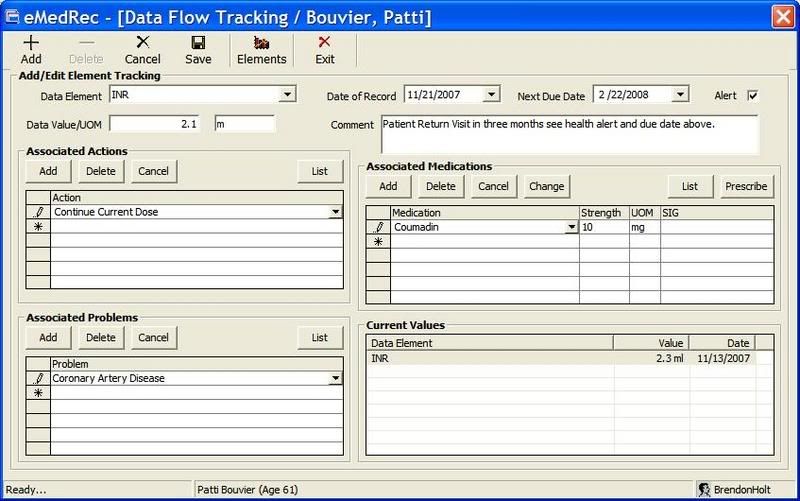
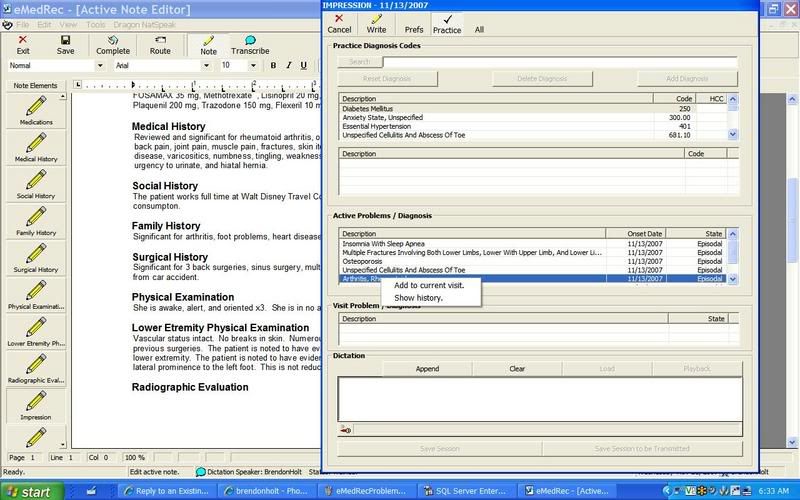
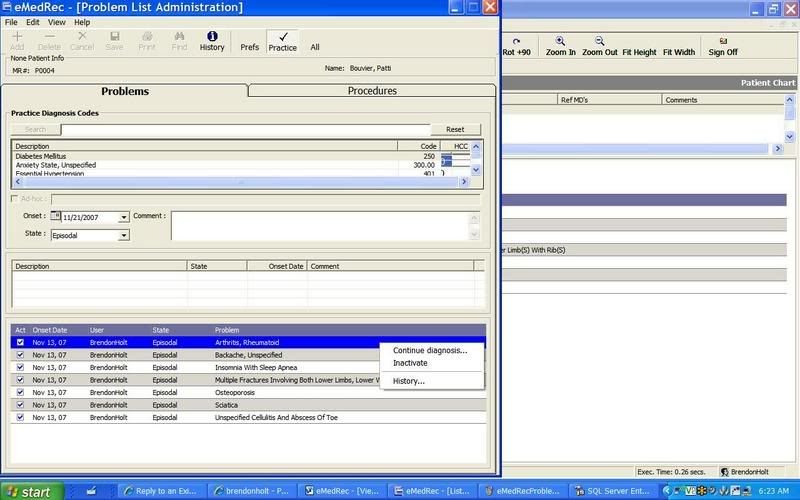
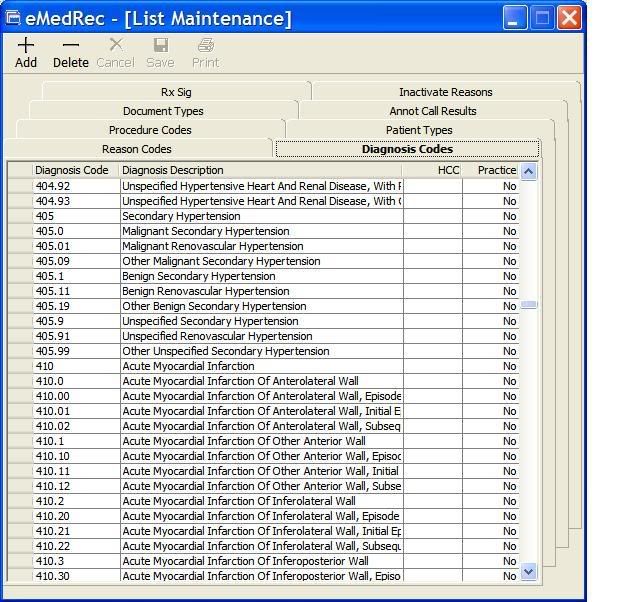
Problem List Management in EMRs
Friday, November 16, 2007
Nursing Home IT
Wednesday, November 14, 2007
Diabetes Disease Management
Here is a diabetes blog with good information on this topic thats worth looking up.
Business Intelligence: Qlikteck in action
Sports, especially football and baseball with their wealth of statistics, are a great application of business intelligence.
Monday, November 12, 2007
Document Management Resources
ScanGuru, a collection of Document Management information. I found this site to have a wealth of information on document management
Intelligent Routing
Sacnners:
From ScanGuru, Network Scanners: evaluations of 3 network scanners. Price range is $2000-3000. Network scanners allow scan to email, network folder or network fax.
Kodak Scan Station 100: High Volume Network Scanner
- A review of product here.
- Scans direct to search-able PDF, TIFF, folder on network, email or to USB drive.
- Cost approx $2200-2600
- Daily scanning Volume of 1000 pages/day
Document Management Solutions
SpringCM a "SaaS" document management solution
1/14/2010: CVISION, OCR software. Can use for PDF conversion, can watch a folder for changes. Looks like a great product. Can download eval software. I will add more once I test drive it my self.
1/14/2010: Interesting stats on document imaging here. Also see this.
Thursday, November 8, 2007
RHIO Resources
Thanks to Christina for these links:
HIM Principles in Health Information Exchange (Practice Brief)
AHIMA HIM Priciples in Health Information Exchange, Case Scenarios good discussion on MPI, typical use cases. Has some nice diagrams
Continuity of Care (CCR)
Learn more about the Continuity of Care
Update on the CCR Standard TEPR 5/2007
AAFP Center for Health Information IT Has CCR resources
HIMSS Electronic Health Records Vendor Association
"The Continuity of Care Document Quick Start Guide (QSG) is provided free of charge by EHRVA, as a service to vendors and others who will be implementing healthcare documents based on the CCD" : Continuity of Care Document (CCD) Quick Start Guide
Visible Body
Wednesday, November 7, 2007
Yahoo, Google and our Privacy, what's there to fear?
"...Yahoo chief under fire over Chinese dissident ...". Apparently Yahoo provided personal Email data from a Chinese dissident that led to his imprisonment . It really should make you think about just how much of our personal information is out there and what some of the consequences can be when our privacy is compromised.
And just today, I also just read about the Candid CIO's enthusiasm about Google's new StreetView:
"Only a nerd like me would be excited about this"
"It allows you to see 360 pictures of the streets in Google maps. Google has mostly taken pictures of the streets in big cities."
"Yesterday, Just as I was arriving home from work there was a car with a fancy camera mounted on a pole that extended high above the roof. On the side of the car was a magnetic Google sign."
I don't know about you, but I'd get a bit nervous about having Google or any one else having even more info on me. And to think now that we are too also have them keep our personal health records (PHR). We really need to think this through carefully.
Tuesday, November 6, 2007
BizTalk, HL7
hl7-info.com – General HL7 issues, debugging HL7 messages and how BizTalk interacts with the messages
biztalk-info.com – general BizTalk issues, HIPAA related issues
Monday, November 5, 2007
Physicians Required to Implement an EMR
I would prefer if they let physicians buy their own EMRs and not have it subsidized. It will be interesting to see how things work out over the next 3-5 years. Technology is changing rapidly. Microsoft and Google are also getting more into healthcare. EMRs available today may appear ancient compared to the new crop of EMRs coming out over the next few years. Buying an EMR today compared to in a few years may be like buying a DOS based system to a Windows system.
Sunday, November 4, 2007
New Service: Document Sharing
This is a new service that allows users to upload various documents for sharing. You can even embed documents in your web pages as shown below. Think of it like a Youtube for documents.
Medicare Rate Reduction
For more information, take a look at FierceHealthIT, Physicians see expected 10 percent Medicare cut.
Saturday, November 3, 2007
Office Open XML for Healthcare
Using Office Open XML Formats to Support Electronic Health Records Portability and Health Industry Standards
It includes sample code
Here is a description taken from the site:
"Empowering patients and consumers to securely exchange Electronic Health Records is a big debate in the Health industry across the globe. In this article, we discuss some techniques that use Office Open XML Formats and how to embed custom XML formats to exchange data securely. This particular scenario shows the use of Health Level Seven (HL7) Clinical Document Architecture (CDA) to represent the Electronic Health Record in an industry standard format. It also shows how to include the data in a secured document, based on Office Open XML Formats, for portability across multiple care providers."
Our healthcare costs not producing results? My take on this matter
Example: Patients who present with low back many times have the expectation that they will need an MRI. Even if I'm able to convince them that an MRI is not justified in the acute stages of low back pain, if they are not better in the next few weeks, they will demand an MRI. In many cases, the doctor will go ahead and order the MRI at that point. In this low back pain case, the cost of healthcare goes up steeply after the MRI is ordered. Now will there be any improvement in any outcome measures of back pain as a result? Most likely no. Studies have repeatedly shown this to be the case. In fact, for most back pain cases, patients get better with simple, low cost conservative treatment such as back rest.
A similar case of low back pain treated in a third word country would likely have a similar outcome as in this country- the patient gets better after a few months of conservative treatment. In this country however, we will have spent money on countless office visits, MRIs, physical therapy etc, while in a third world country, the only cost would have been a single office visit. So does this mean that our healthcare system has inferior outcomes? No, its just that our healthcare users have a different set of expectations from their healthcare system than in other countries.
As far as "defensive medicine" and costs, when there's an unfortunate healthcare outcome for example, in this country it's automatically assumed in many cases that it's the fault of the healthcare provider. Remember the recent ex-Patriot coach, Charlie Weis's lawsuit? Situations like this natuarally effect the practice of medicine by our healthcare providers.
For better or worse, our healthcare dollars do not all go towards improving outcome statistics. The cost of healthcare, as well as happiness in general, is just higher in this country.
Friday, November 2, 2007
HL7 v3 sample Code from Microsoft
Go take a look at Roberto Ruggeri's blog item: Getting Started with HL7 Version 3 and BizTalk Server 2006 (R2) for more information.
Here is the link to the sample code. Here is the whitepaper on getting started with BizTalk and HL7 v3.
Thursday, November 1, 2007
TeleHealth and HealthVault ?
HealthVault Lays a Foundation to Build Scale for Telehealth
Applications
Today, telehealth applications are based on point to point
relationships: home health agency to patient; disease management company
to patient; health system to patient.
Telehealth devices and their
connectivity are similar. There is a proprietary chain of key components for a
remote patient monitoring (RPM) solution: 1) the RPM device; 2) a gateway
-- which could be mobile like the Biotronik
Cardio Messenger or static like a personal computer -- to aggregate data
from multiple devices and move data to a server-based application; and 3) the
server application that stores and manages the data in accordance with the
application, e.g., glycemic control, medication compliance, etc.
Athena Health Platform and HealthVault? Just me thinking...
The back office "practice management" function (the medical billing) is a far easier nut to crack. Most doctors are already submitting claims electronically (directly or via a billing service). The EMR piece is more of a challenge and in some ways more "art" than science.
My feeling is that Athena Health should spend their efforts more on creating an interoperable "Practice management" platform in the same way Microsoft created Healthvault as a "PHR platform" rather then a PHR application. With Microsoft's approach, PHR vendors will use HealthVault as a backend platform to perform core PHR functions. In other words, Microsoft is not trying to take over the PHR space, but rather be a part of every PHR.
By creating a "Practice Management Platform", EMR vendors may design their systems to integrate with Athena Health's practice management functionality (this is done via a set of web services). The reason I say this is because those who know EMRs best are not the same people who know practice management functionality. If I was to design an EMR (which I am doing BTW), I'd much rather integrate well with a solid Practice management system than design my own.
Thin vs Thick Client and Microsoft's Smart Client
Thin vs Thick clients is always a great discussion. Microsoft has the "Smart Client" platform which is essentially a thick client UI that uses web services on the back-end to connect with the data-store. This has the benefit of allowing the "Smart Client" application to work in distributed environment, just like a typical web application.
The "rich" windows UI of the Smart Client is the advantage over a web UI. Ajax however is making web applications look more like a rich Windows-like UI. Just check out, for example, the new Yahoo mail (my personal email platform).
The Smart client distinguishes itself by allowing for an "off-line" mode, which is great in scenarios where Internet access is not always available. Installation and deployment however is the downside of the Smart Client, although it has been made easier with this platform. This is where pure web applications shine.
I wonder if Microsoft is still committed to the Smart Client now that they have another UI platform in the works, code name "Silver-Light", which will further bridge the gap between a Windows and Web UI. We'll have to just wait to see how things sort out in the end.
Wednesday, October 31, 2007
Privacy Advocate supporting HealthVault?
But seriously, listen to this interview for a viewpoint of a real patient privacy advocate, Deborah C. Peel MD,MD. Also, see their website.
Another HIE related failure
Unfortunately this is another case of an HIE or RHIO living off grants only to find out later that there's no true sustainability model to keep it going after the initial grant funding dries up. No one felt there was enough value in the HIE to justify further investment.
With many HIEs, its always easy to use someone else's money (i.e, government funding) to get things started. These efforts always begin with high hopes of all kinds of benefits to patient safety, cost reduction, greater efficiency etc. Somehow, when its time to use your own money, these benefits don't seem worth it. My feeling is that many of these HIEs are set up as huge bureaucracies, with all the "C's"- CEOs, COOs, CIOs. There really is no way an HIE can support this type of boated infrastructure. HIEs really need to be "lean" in order to succeed.
Friday, October 26, 2007
Healthcare Business Intelligence
What I like about this company's approach is that they allow you to download a trial version of the software. I downloaded the trial version a few weeks ago and must admit it was very easy to get things up and running. I hope to spend a little more time with the trial software later. I am curious however to know the cost to license the software.
PriMed East Boston follow-up
The Hynes site was much move vibrant due to its presence in the Boston. The new convention center in contrast seems to be in the middle of nowhere, tucked in the midst of warehouses and other industrial buildings. I do hope PriMed organizers take notice and return the conference to the Hyne's.
Thursday, October 11, 2007
Open Source EMR
The design of the UI is based on the classic MVC pattern or the Model-View-Controller design pattern. If you're interested in how to implement the MVC pattern in .NET, look at this.
There is an architecture document, but is seems a bit sparse. It does at least show the organization for the project.
The best part is the data model, which is provides a fair amount of detail. It follows a fairly classic healthcare data model for "Patients", "Orders", "Medications" and "Laboratory" entities.
All in all, it looks like fairly neat project. We need more such open source efforts to make the adoption of health IT more affordable. I hope more independent and highly motivated developers take the plunge and really do for Healthcare IT what they did for personal computers and software in the 1980, and the Internet in the 1990's. We can't allow Healthcare IT to be monopolized by the big companies.
PriMed East Tomorrow
I'll be sure to give a run down of the event next week...
Wednesday, October 10, 2007
HL7 v3, A Challenge in Implementation
I've spent a lot of time trying to implement a practical HL7 v3 solution. I quickly realized that to use it for messaging would be highly impractical. There are just too many possible interpretations of how to convey a message using the v3 messaging model. A great quote I remember describing HL7 v3's XML structure, was "they used every trick in the book".
What I did find helpful however was the RIM (Reference Information Model) as a health-care data model. Having said that, I would caution against using the HL7 v3 RIM to model a logical relational database design.
RIM can serve as a very useful starting point for a design, but do not use it too literally. Doing so can lead to a very inefficient and needlessly complex database design. As I learned in engineering school, learning where to make trade-offs is the difference between a practical design and an exact, but impractical design.
Monday, October 8, 2007
Nursing Homes finally getting attention
There is a complete lack of any IT at most nursing homes. Patients frequently come from multiple sources, such as community and tertiary hospitals. Patients bring with them stashes of paper-- labs, radiology reports, discharge summaries etc. Trying to put all the information together to get a complete view of a patient is nearly next to impossible. It is at the nursing homes where IT- RHIOs/HIEs and telemedicine can have a real impact in the quality of care of patients.
I'm happy to see long-term care finally get some attention.
Likely PHR users
The vast number of PHR users are likely going to be the "worried well" (hypochondriacs) or those people with chronic illness who like to track (or in some cases, obsess) over their health issues.
The elderly, who probably would have the most to gain from a PHR for its ability to track long medication lists, multiple doctor visits and hospitalizations, are the same people who would be less likely to use a PHR. And this is not just because the elderly are not computer literate, but because of the usual age related health problems, such as low vision, early dementia etc. We will need to depend on the care givers to manage their PHRs.
To most people however, healthcare is something they hire someone else to worry about (the doctor) in much the same way we have a fund manager to manage our mutual funds. I suspect that it will be the “Quicken” types who will make up the vast majority of PHR users.
Sunday, October 7, 2007
Obstacles for PHRs, HealthVault?
" "Consumers are just not that excited about these" services, said Elizabeth Boehm, an analyst at Forrester Research Inc"
"Few households watch their health closely, so they aren't looking for new health tools. "In general they're not tracking it and don't understand the value of having it equally shareable" in digital form, Forrester's Ms. Boehm said. "They just don't understand what's in it for them.""
I must say that I do agree that most patients are not interested in this detailed level of their healthcare. The PHRs are being promoted/marketed to the general population, while products such as EMRs (electronic medical records) are targeted at a smaller group, the physicians. If just 10% of the population adopts PHRs, this may be considered a success from a consumer business standpoint, but will not necessarily revolutionize how healthcare is practiced. Wide-spread physician adoption is still the key to any healthcare revolution.
Unfortunately, those that consume much of the healthcare resources, the elderly and less affluent, may be less likely to use a PHR. Most PHR users likely will be among the better educated and many of these people will be the so called "worry-wells" (patients that are actually health but worry about their own health disproportionately)
Saturday, October 6, 2007
Microsoft HealthVault for storing our data, Issues regarding Privacy and Security
The only people that really might have an interest in my health data would be my family, friends, neighbors or co-workers. One can argue that my employer may as well. The real fear however would be if the government or insurance companies get access to my PHR data. If thats the case, they would not do it illegally by hacking (as would a neighbor). I'm afraid this would only happen if we allow a shift in public policy to take place which would permit our PHR data to be accessed by these other entities.
Once there is a sizable PHR database based on our nations population, it will be too tempting for politicians and policy makers not to try to make arguements to justify use of this data for the "public good". As politicians frequently do, they'll say, "we're doing it for the children".
This is the real threat to the privacy of our data.
Google's PHR
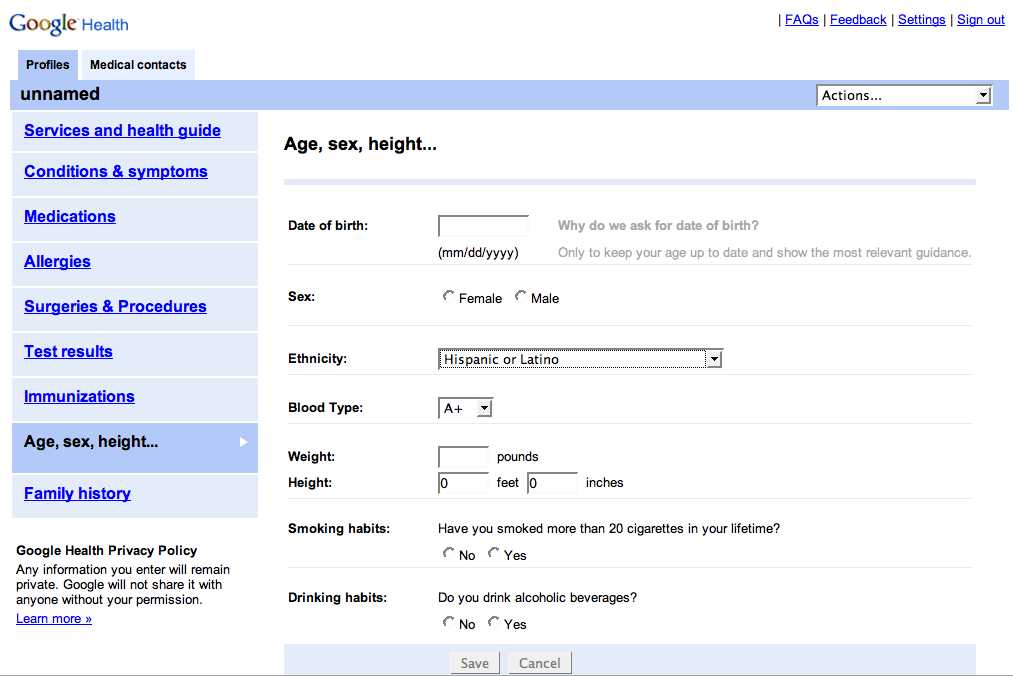 While on the topic of HealthVault and PHRs, the discussion would not be complete without mentioning Google. Here is a link to some screen shots of Google's prototype PHR. This is more of a PHR than Microsoft's Healthvault. My patients and fellow physician colleagues would not have a problem understanding this type of application, its functionality is very obvious. Google's prototype PHR appears to be an "end-product" rather than a set of services like HealthVault.
While on the topic of HealthVault and PHRs, the discussion would not be complete without mentioning Google. Here is a link to some screen shots of Google's prototype PHR. This is more of a PHR than Microsoft's Healthvault. My patients and fellow physician colleagues would not have a problem understanding this type of application, its functionality is very obvious. Google's prototype PHR appears to be an "end-product" rather than a set of services like HealthVault.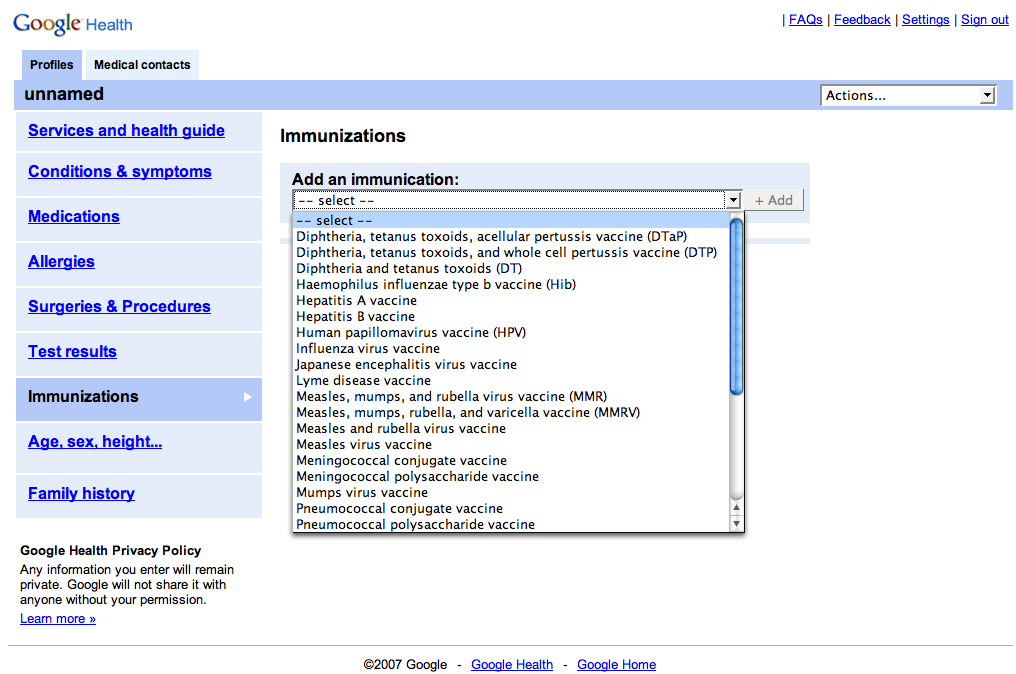
Part III: Understanding how to Develop Applications with HealthVault
What does HealtVautlt mean to me as a developer? How does it work?
Here is the scenario as I see it, which explains how a developer may start to think of ways to use HealthVault:
Developing with HealthVault
- Lets assume a patient, John Doe registers for a HealthVault account. This is where his healthcare data would be stored. John Doe controls access to this data using his "Windows Live ID" credentials (user-name and password).
- Now suppose, I as a developer create a new PHR product called "Acme PHR" using HealthVault on the backend. That is, I develop the presentation layer, the actual website with my company's logo etc. I decide the look and feel of the application and the type of data I want want to collect and store for a patient. Additionally, I would also develop the business layer containing the business rules, knowledge-base and decision support functionality.
The final Acme PHR product is my company's application. The application performs the functions that I want it to perform. I can do interesting things with the application by combining the data in HealthVault with additional data that I define and store separately on my own server/database.
Designing a new HealthVault-based application- Personal Diet Planner and PHR
What do I mean by combining HealthVault data with my own defined data? Lets take an example. Suppose I want my PHR application to have the ability to provide different diets for patients with various health conditions, like diabetes, hypertension or obesity.
With my PHR, I will want to collect patient data such as weight, blood pressure, health conditions, blood sugar values, cholesterol results etc. This data is patient specific, so I decide to use HealthVault as the storage mechanism. Besides the convenience of using HealthVault's APIs, the big advantage of HealthVault is that it handles all the security issues, such as authorization and role based access to data (specified by the patient).
The database of the different diet plans however is stored on my company's servers. It is my company's proprietary data and would be kept entirely separate from HealthVault's data.
With my application, I can combine patient specific data from HealthVault, with my database of diet plans. So if a patient using my PHR, has high blood pressure and is obese, I may recommend a particular diet plan, while someone with just mild obesity, may get another diet recommendation. This is my application's "secret sauce", the ability to decide the proper diet for specific health conditions.
This is an important point, because my application is not about the details of storage and retrieval of health data, but rather, on how I use this patient's specific data and combine it with other data to create new innovative personal healthcare applications. This is much like an operating system. HealthVault essentially acts as an operating system like Windows, handling all the low level detail and chores, while my application focuses on the big picture.
Whats next? More Applications using common HealthVault Data
So patient John Doe uses my "Acme PHR" (with the special diet plan feature), and has entered his health data. John Doe is very happy with my PHR product.
But now, another company creates another product using HealthVault which recommends exercise plans for patients with specific health conditions. John Doe likes this idea. He has all his data already entered via my PHR product and is happy with the diet plan. He now wants exercise recommendations. John Doe can subscribe to this new "Exercise Planner" application. Fortunately, because it too uses HealthVault, John's data is already entered. This data can now be used by this new application. So using John Doe's existing weight, blood pressure and health condition data, an exercise plan can be recommended by this new product. There can be other products which do other things. The possibilities are endless.
HealthVault is like an Operating System
You can see the tremendous advantage of having personal health data stored once, with the ability to use it in multiple ways with disparate products. Just as the Windows operating system has resulted in countless software products, HealthVault likewise may lead to countless health care applications.
Friday, October 5, 2007
PHRs, too much Hype?
Part II. Microsoft's new HealthValult, More thoughts
I was hoping for a robust PHR. In fact, I was hoping to start signing up my patients for accounts as they presented for their appointments. However, if I found the application confusing, it would be pointless trying enroll my patients at this point.
I looked up all the available information on HealthVault from the Microsoft site. Because of my experience in developing healthcare applications, I believe I have a fair understanding of this application now. However, for many, I believe the application is a bit obtuse. I think it's fair to say, HealthVault, despite a barrage of news in the popular media, is not quite ready for direct patient use.
I do remain excited by this offering despite my early disappointment. Having a large company like Microsoft leading this effort, I believe there will be more opportunities for independent developers to create new healthcare applications. I know many think Microsoft is trying to "take over" healthcare, but I'm trying to take the positive view. We'll just have to wait and see.
More on HealthVault later...
Thursday, October 4, 2007
Microsoft's new Health Valult, a PHR?
As a practicing physician, I'm really excited about this application and have signed up for a personal account. My plan is to start enrolling my patients with the hope of consolidating their medical data.
I found however that the application did not have a place for me to enter my past medical history, medication lists etc. I think, for this application to work for my patients, this feature needs to be in place. Perhaps this feature already exists. If this is the case, it needs to be more obvious to the user. I know this is in beta, so I'm willing to wait. My hope is that the Health Vault is a true PHR.
There is an interesting integration feature. I can fax documents to my patient's account using a fax subscription service that converts the faxed document to a PDF file for storage in the patient's Health Vault. The patient must subscribe to the service. The cost is very reasonable however.
I will write more about the HealthVault as I discover more of its features.
Results Managemenent, Critical results reporting
Although many times these critical results are also faxed to the doctor, this really is not an acceptable way of communicating a result needing follow-up. Faxes are notoriously problematic. You can never be sure that the recipient has received the faxed document. After all, fax machines can run out of paper or ink and there is no way for the sender to know that the recipient has received the document.
There needs to be proper follow-up on abnormal test results. By this I mean the radiologist making the abnormal finding should really be calling the ordering physician to review these abnormal findings and to develop a follow-up plan. When results are very high in critical severity, this process usually occurs. When the results may not rank high in the severity scale but are still abnormal, a one-to-one notification method still needs to be in place. There needs to be a system to verify that the abnormal result was received by the appropriate party. An electronic system would be ideal.
If an abnormal result has not been receieved by the appropriate provider, another attempt must take place to convey the results. If all attempts fail, there needs to be further escalation of the process to ensure that a responsible physician is able to act on the abnormal results.
I came across a possible vendor solution to this problem:
"Critical test reporting, closing the loop"
http://www.vocada.com/veriphy-solution.asp
Wednesday, October 3, 2007
Learning from Past HIE / RHIO Mistakes
Here a few quotes from the article:
"pioneers in this emerging field concentrated on creating entities, not functionality. " "... they set out to build an organization like a RHIO, rather than advance the attainment of information exchange. "
I have been commenting on this point of how RHIO have been all about setting up large organizations rather then entities that actually do something useful from the physician user perspective.
Another great line from the article:
"With the focus on form, not function, it was easy for participants to get sidetracked with political agendas, competing priorities and administrative processes..."
This reminded me about a recent encounter at a healthcare conference recently, where I met the head of a major EMR vendor's community based initiatives group. While discussing our RHIO initiative, SEMRHIO, I was asked by this vendor representative,"What is your governance model". I smiled and told her, " Our model is about creating real value for the physician , not about by building an organizational structure".
I believe in the "If you build it, they will come" model. Like any great invention, its the idea that comes first, then the organization. After all, Thomas Edison's light bulb came before General Electric.
With RHIOs, we need to focus on "what do our physicians need to enable them to care for their patients?". This should be the guiding principle. It usually takes several iterations to get the right model. Too many development initiatives get locked into a model from the start. RHIOs need to be agile, and have the ability to change or modify the model if required. By having something people really want, the rest should come easy.
Tuesday, October 2, 2007
Physician Mobile Device Applications
The problem however is the fact the physicians also need to access a vast array of detailed data when taking care of patients. The challenge with these applications has been with making the data easily accessible on a small mobile device and to do it in an efficient manner so as not to be awkward to use.
There are several very useful applications currently available for the mobile device. The Epocrates (http://www.epocrates.com/) drug data base is probably the most popular application designed for the mobile platform. As a physician, I always have it on me and constantly use it all day long.
Another application, that I feel will be very successful, is the mobile platform for medical education/CME/Case consults by QuantiaMD . What I like about this application, is that as a busy physician on the go, I can listen and watch interesting medical content by Quantia on my Motorola Q-phone. This content can be tailored by Quantia to come from my affiliated hospitals, such as hospital grand rounds. Physicians from my healthcare community can post interesting cases and do short powerpoint presentations which I can access on my mobile device or via the web.
I'd be interested in hearing about other mobile applications.
Friday, September 28, 2007
RHIOs Should Exist to Enable Critical Data Sharing
"I certainly like the idea of data following me. I love the idea of my providers cooperating. But at the moment, I simply can't see how this kind of data sharing can work in the near future."
Well, patient data sharing is not some novel concept that needs debating. Its already happening, although some do not even realize it. It happens by the fax machine. Patient data sharing is an essential function of caring for patients.
Replacing the fax machine, an inherently in-secure method of data exchange, by a secure electronic exchange is what a RHIOs should be all about The discussion should not be about whether RHIOs should exist, but rather, what is the best model for a RHIO in order to win trust among entities to enable clinical data sharing to take place.
We made a case recently at the recent MSHUG fall Forum 2007, for a RHIO Trust model, which has been very successful in gaining trust among our participants in SEMRHIO.
Thursday, September 27, 2007
Medical Home, a case of the “Emperor’s New Clothes” ?
So far, what I heard, the medical home concept sounds awfully similar to the concept of the “HMO Health Center” of the 1990’s with the addition of EMRs.
“…continuous care, coordinated care across the health system, utilization of information technology and enhanced care through systems such as open scheduling.”
“…the concept of partnerships between primary care physicians and patients to coordinate access to all needed medical services and consultations (a 'medical home') for all patients."
In the “HMO Health Center” model, the PCP was the “gate-keeper” or care-coordinator. From my experience in managing an “HMO Health Center” during its final days in 1999, we had our own case managers and social workers who helped coordinate the care of our patients. We followed the care of our patient’s from the ambulatory setting, to the hospital, and then to the return to home. We worked closely with our “contracted VNA” (Visiting Nurse Association), hospital case managers, and nursing homes. We had our panel of preferred specialists who helped care for our patients.
What we did not have however, was an electronic medical record or a community health information exchange. I remember being frustrated with not always having right clinical data when I needed it. As a former engineer, I knew then that clinical data access was the one thing that was truly lacking and prevented us from achieving the promise of the HMO health center model of safe, efficient and patient friendly healthcare.
Well, with EMR and health information exchange technology (or RHIO), I hope the "Medical Home" does not turn out to be a case of the "Emperor’s new Clothes".
If you are trying to understand the Medical Home concept, check these :
Medical Home Concept Catching on in the US a Washington Post Article
Medical Home Concept Paper An in depth paper from the state of Louisiana
Waye and Means, Medical Home
eCareManagement Blog item on Medical Home
The Patient-Centered Primary Care Collaborative : coalition of major employers, consumer groups, and other stakeholders who have joined with organizations representing primary care physicians to develop and advance the patient centered medical home.
Wednesday, September 26, 2007
Performance Reporting on Lab data
If batch reporting is your main need, the CALINX Lab import tool may be for you. It converts HL7 v2.x lab data to a "flat-file". A flat file is essentially just a comma-delimited data file. Most "MS-Access" programmers are familiar with importing this type of data file into a database. Its certainly easier to work with lab data in this format. Check out the Calinx guide, which provides a very straight forward description of the Calinx lab data standard and provides an excellent primer on HL7 v2x lab data.
RHIOs are still relevant according to Dr Brailer
Dr Brailer still remains bullish on the prospects of RHIOs. He admits that RHIOs are undergoing a shakedown. I also believe this is the case.
Take the dot-com boom as an example. The initial exuberance was followed by people questioning whether the Internet could actually produce a sustainable business model. Well, since then we have seen the likes of Amazon.com, Google.com, youTube.com, and the list keeps growing.
RHIOs too, I believe will follow a similar path. Just as with the dot-coms, when funding was abundant, there was a "spend-spend" mentality without regards to sustainability. RHIOs, like the dot-coms, had been flush with significant funding, mainly from state and federal grants. In fact, there is a term for these grant-dependent entities: "Beltway bandits – a group of people who live off government grants", "grant babies" (see HISTalk)
The Santa Barbara RHIO is a good example, where it did not take long to burn through $10M in funding, only to learn in the end, that there really did not seem to be a need for such an entity in their community. Just recently, we learned of the shutting down of the Oregon RHIO, which did so only after spending nearly $500K just to find out that their RHIO was going to be to expensive.
Once you start hiring those consultants and lawyers, and start setting up committees, money can dry up very fast. RHIOs need to evolve, I believe from an entrepreneurial model that enabled the small technology start-ups in the 80s and 90's to beat the larger companies. After all, it was this model that allowed IBM to develop the now famous IBM Personal Computer (IBM-PC). IBM, in the early 80s, after learning from the success of Apple Computer, used a "small start-up company" model to develop the IBM-PC.
RHIOs will start to succeed once they focus on sustainable models that meet true business needs rather than needs decided by committees. They will need to adopt a "start-up" model, depend less on government funding (handouts), and rely more on self-funding and private investments.
Tuesday, September 25, 2007
More new on ICU Telemedicine
AMA News: Big hospitals adding remote monitoring for ICU patients
The article describes the e-ICU implementation at the University of Massachusetts Memorial Medical Center. VISCU, an ICU telemedicine systems company that I described in an earlier post, is the apparently the only vendor selling such systems. The article states that more than 200 hospitals use it to monitor 250,000 patients a year.
Some of the drivers for ICU telemedicine is the growing physician shortage and new patient safety initiates. I can certainly can testify to the fact that with the increased emphasis on patient safety, and the new medicare policy for "no payment for medical errors", we will see the growth of telemedince and other advanced monitoring technologies.
Some of the benefits seen from introducing ICU telemedicine at the UMASS Memorial Medical center were:
1- decline of pneumonia rates
2- decrease in deaths by 9%
3-decrease in length of stay
4- decrease in ventilator-associated pneumonia to 1/4th the national average.
These results are impressive. If they also translate to cost savings or increased patient volume, more hospitals and other healthcare facilities will be incentivized to further adopt telemedicine services.
Friday, September 21, 2007
Discussing Healthcare data exchange on Deb Zona's "Healthcare in Crisis" show
The purpose of our discussion was to describe in very simple terms, the problem that is faced by physicians, patients and care-givers in trying to keep track of a patient's clinical data including medication lists. We used this discussion to serve as a laymans introduction to the concept of a RHIO or HIE.
Clip1
Dr Maggio discusses Medication Reconciliation and how patients manage their own medication lists.
Clip 2
Some points discussed:
Clip 1:
- Patient clinical data is spread out throughout the community, at the various hospitals, imaging centers, labs etc.
- Patients in their healthcare, can undergo multiple care transitions during their illness. These transitions may include home to hospital, to nursing home/rehab, to home with VNA and finally back home under previous arrangemnt.
- Challenge for the physician and the patient/care-givers, is keeping track of the data that is generated at each of these care settings. It is critical not to lose track of any data as care settings change.
- It is importany to maintain a unified view of the patient regardless of the care setting.
Wednesday, September 19, 2007
Home telemonitoring, new study released
Here is what was said:
"Home telemonitoring of chronic diseases appears to
be a promising approach to patient management, says a team of Canadian scholars
who reviewed more than 65 telemonitoring studies in the United States and
Europe..."
"The 65 papers they examined included studies on
the home-based management of chronic pulmonary conditions, cardiac diseases,
diabetes, and hypertension. Each of the studies employed various information
technologies that were used to monitor patients at a distance.
"
"The study, entitled “Systematic Review of Home
Telemonitoring for Chronic Diseases: The Evidence Base,” appeared in the
May/June 2007 issue of the Journal of the American Medical Informatics
Association. "We need more studies like this to generate interest in this area and to really help telemedicine become a "standard of care".
Telemedicine in Diabetic Disease Management
See this article: "Trend: Managing chronic diseases remotely, with mobile tech":
"HealthPia's GlucoPhone, which combines a glucometer with a cell phone, is being used by fewer than 100 patients nationwide since FDA granted it premarket approval last year. HealthPia charges $79 as part of an introductory package for its GlucoPhone, as long as patients also pay for the service from its selected
telephone carrier, LogicMobile. Patients also have to purchase testing strips
that must be used in conjunction with the phone, although Medicare reimburses
patients for the strips."
Telemedicine in the ICU

I just came across some good links on Telemedicine ICU applications:
Check out the Doctors who developed the use of an ICU Telemedicine system used at Penn developed by a company, Visicu, the "eICU system" (Visicu, like "Visual ICU") .
Take a look at their technical architecture diagram.
Notice the similaries with RHIO technical architectural diagrams. Same HL7 challenges etc. Again, I see Telemedicine as a natural extension of disparate clinical data integration challenge.
In an earlier post, I mentioned how, because of lack of payer reimbursement for telemedicine, the costs may be borne out by facilities such as hospitals because of a perceived notion that telemedicine brings better outcomes and as a result reduced costs. This is apparently the case at Penn's Telemedicine ICU:
Doc in a Box blog writes:
"And also we must not forget about whether we can
bill for this service. Presently the hospital supports it based on the notion
that increased quality saves money."
The Telemedicine Market
Broadband where it’s never gone before and other technological marvels
by Jonathan Blum, April 2007 issue
"The Ultimate UCG: Telemedicine
Think user-created video
and music are hot? Meet telemedicine.
Sometimes called digital medicine
or remote monitoring, the process of providing health care remotely via the Web
is a massive market that is finally beginning to organize.
Around 60 million
people in the United States suffer from a chronic illness, according to
Dallas-based research firm Parks Associates. Factor in those providing care and
the total audience for health care can easily double, or even triple, that
figure.
With the potential audience that high, the telemedicine market is
expected to grow to $1.83 billion by 2010, according to Parks Associates’
research analyst Harry Wang. And companies like adt’s QuietCare and Webvmc are offering services such as remote
monitoring, in-home wellness, and the Remote Nurse — a purpose-built health-care
display.
“The technology behind the industry has been in place for 15
years,” says Wang. “What holds it back is the lack of
understanding of the business between doctors, insurers and patients.”
In other words, a few good branding campaigns
could help this nascent industry grow into a real market. "
The real challenge that I have found is exactly the physician-business part. The "doctor's business" is very different from any other business. It is not strictly a consumer-driven, price sensitive business. We have third party payers, the insurance companies, which tend to drive healthcare spending depending on what services they cover and the reimbursement amount. I do not expect patients to pay for these telemedicine services themselves. More likely, it will be the payers or healthcare facilities, such as hospitals and nursing homes that would pay for these services if they see some improved outcome or cost saving.
The promise of telemedicine is delivering timely healthcare that meets the demand of the patient's illness. Similar to the concept of the "on demand service" concept that we see in the general IT space. With more timely medical interventions, patients would experience fewer treatment delays, less complications and thus reduced overall costs. If we can make this case, I'm sure we'll see the payers move faster in this direction.